|
Exercises to help prevent Occupational Overuse Reference: Developed by Sentinel Supported by ACC
If you are experiencing pain or discomfort doing your job out friendly physiotherapists and occupational therapists can help. Just contact us Phone: 03 377 5280 Email: admin@tpl.nz Physios key to shorter waitlists (Article from The Press, January 19, 2024)  Lynn Downes doesn’t need prompting to get up and dance. The 73-year-old has spent the holidays running around after her seven grandchildren despite, a year ago thinking she might have been facing a hip replacement about now. Downes had her right hip replaced in 2021, then her left side began playing up a year ago. “I thought, ‘Oh, gosh, here we go.’” It had taken two referrals from her GP in 2021 before she was scheduled for surgery. Her pain had worsened, and she didn’t fancy joining the treatment queue again. That queue has been an ongoing headache for Te Whatu Ora-Health NZ. As of November, more than 1500 people had been waiting more than a year for orthopaedic treatment. Traditionally, the standard treatment process meant a patient referred by their GP went straight to an orthopaedic surgeon to be assessed. Now a Wellington pilot allowing orthopaedic physiotherapists to assess patients in the first instance has reduced treatment times by an average of 75 %. In Wellington, patients are now waiting an average of 40 days for an initial spinal assessment, rather than 180 days in December 2019, while hip or knee complaints are being assessed in about 45 days. In August 2021 these patients were waiting 165 days. Downes admits she was sceptical of the approach at first, but the exercises have allowed her to sleep without pain and keep pace with her school-aged grandchildren. “She went over my history, the X-rays…She gave us some exercises and a pathway so I could contact her if my symptoms got worse,” Downes said. “It’s a much better route. If things got worse, the physio would then contact the surgeon.” Her treatment is ongoing, but she said she hoped to avoid surgery. In Wellington, the pilot has been led by expert physiotherapist Sarah Francis, who said more than 600 patients had been through the programme since September 2022, at Wellington and Kenepuru hospitals and Kāpiti Health Centre. Of course in some cases, surgery would be unavoidable, Francis said. But there was no need for every patient’s first assessment to be done by a surgeon. “Part of this project is about making sure people get non-surgical care earlier. The sooner we intervene for people with, particularly conditions like osteoarthritis, we can prevent progression to joint replacement,” Francis said.  Patients were happy, too – 86% felt confident in being assessed this way, and fewer than 5% were referred back into the system after one year. Last August, Te Whatu Ora said it wanted to treat all orthopaedic patients who had waited more than a year by June 30. This was still the goal, planned care and cancer programme director Ian D’Young said, and good progress was being made. It was forecast that more than 14,000 patients were in that category, and by December 3 that number had come down to 5,222, he said. But for some it’s too late. Wellington man David Garlick, 25, was turned away from the public system after two years of bouncing around appointments seeking help for a condition causing painful excess bone growth on a femur. For him, surgery was unavoidable, but the time spent languishing in the public queue meant his condition worsened, taking an enormous toll on him and his fiancé. “It was a waste of my time, their time, everyone’s time.” It also left him facing $30,000 private medical bill, only avoided after a surgeon from the Auckland-based Aotearoa Charity Hospital read about his ordeal in The Post and offered to operate for free. Garlick now needs the same surgery on his other hip, which he also hopes to get done through the charity hospital. D’Young said Te Whatu Ora appreciated the impact of treatment delays “and we are working hard to put in place systems and processes so improvements to waiting times are made”. Author: Rachel Thomas, The Press, 19 January 2024 Efficiently cleaning an aged care environment Cleaning is an essential part of the prevention of healthcare-associated infections. Contact with contaminated surfaces or objects in aged care environments can cause infections. So how do you keep an aged care facility clean? Preparing the cleaners’ trolley Upon arrival, cleaners consult the table of products and the protocol for alternating between detergents and disinfectants. Some rules are immutable. Gloves are mandatory for all contact with products as part of the cleaning standards. Never mix cleaning products because this can create dangerous chemical reactions. When using dilution equipment, ensure that it is well-maintained and kept in good condition. Always refer to the manufacturer’s instructions and renew cleaning solutions accordingly. Observe the temperature and contact time indicated. Cleaners and in aged care facilities prepare their trolley by selecting the equipment that they need to perform all the care services scheduled tasks. Staff use equipment that is in good condition, clean, and in compliance with safety regulations. Organising the trolley is as follows:  Put the cleaning equipment at the top. This includes cleaning chemicals, disinfectants, sprays and wipes.
Standard method in bedroom maintenance in aged care facilities Hand hygiene is essential before cleaning, after cleaning, and whenever it is required, especially in changing gloves. The care environment for the aged care setting is crucial.
 Flat mopping Like any washing procedures in a cleaning aged care facility, flat mopping is preceded by wet sweeping. The flat mop relies on a chemical and mechanical action to remove the dirt adhering to the floor and microorganisms they carry. When using a detergent disinfectant, there is also a specific disinfectant action. This gives visual and microbiological cleanliness. The technique is the same as for wet sweeping. The cleaner began with the most distant part of the room and performed semi-circular movements. The mop is removed at the door. Cleaning in aged care facilities is effectively done in the progressive method. It is by verifying the correct operation of equipment to be left and be placed in aged care facilities. Moreover, some tasks constitute more in-depth maintenance which requires planning. This includes the vents, tops of wardrobes, or the thorough cleaning of beddings. Cleaning staff are needed to brush sanitary installations and wooden furniture. Cleaning in aged care set up can be challenging but rewarding. Imagine your contribution to the health and wellness of our seniors. Author: Beau Sleeman, Clean Group Aged Care New Zealand Issue 02 2022 A window to the brain: The retina gives away signs of Alzheimer’s disease and could help with early detection. The retina has long been poeticised as the window to the soul, but research now shows it could be a window to the brain and act as an early warning system for cognitive decline. A growing body of research suggests the retina is thinner in people with Alzheimer’s disease reflecting the cell loss that is a hallmark of the neurodegenerative disease. We investigated a group of middle-aged people who are part of the Dunedin study, a comprehensive longitudinal project that has continued for five decades. We found people with thinner retinal nerve fiber layers (one of the cell layers in the retina) had slower mental processing speed. This is one of the first cognitive processes to decline in Alzheimer’s disease. The people in our study were 45 years old, which is young for investigating age-related neurological diseases like Alzheimer’s. But treatments and interventions are most effective when administered during the earliest stages of Alzheimer’s and it is crucial to find ways of identifying people’s risk as early as possible. Easy risk identification will also help with clinical trials for Alzheimer’s disease treatment.  Why the retina is a good biomarker for the brain Many of the processes that happen in the brain also occur in retinal ganglion cells, another layer of cells that make up the retina. This includes some of the abnormal processes common in Alzheimer’s disease, such as the abnormal deposition of amyloid beta protein and cell loss. Retinal imaging has many advantages over the other imaging technologies. It’s fast, with each scan taking only a few seconds, non-invasive, painless and relatively cheap. It’s also widely available. In Aotearoa, every hospital eye department has an optical coherence tomography (OCT) device for imaging the retina, and these devices are increasingly available in primary care clinics and retail optometrists. Retinal imaging also lends itself to being interpreted by artificial intelligence applications. This means assessment of Alzheimer’s disease risk from the retina could be quick, easy, and widely available. For these reasons, researchers are beginning to investigate how early the retina starts to thin in Alzheimer’s disease. The disease has an insidious onset with a gradual decline in cognitive processes such as memory, but the underlying pathology tends to be fairly far along by the time people notice the symptoms and seek medical treatment. If we can detect retinal thinning before the symptoms become apparent, it could be possible to identify people who are in the earliest stages of Alzheimer’s disease.  Retinal thinning and cognitive decline in middle age The people we studied are all part of the unique Dunedin Study, which tracked the development of a thousand babies born in Ōtepoti Dunedin between April 1972 and March 1973. They’ve been assessed repeatedly every few years since, on a wide range of topics including mental health, risk-taking behaviours, respiratory and cardiovascular function, social support and dental health, among others. They’ve also repeatedly undergone cognitive tests since they were children, each time using similar formats and standardised tests. This means we can compare their cognitive performance in middle age with their own results from childhood. Most cognitive tests used in Alzheimer’s studies are blunt tools designed to detect large drops in cognition. But the detailed cognitive data we have allow us to detect even small cognitive changes. Using statistical techniques, we used each person’s cognitive scores in childhood to predict what we’d expect their cognitive score to be at age 45, and measured how far away they were from what we’d predicted. A number of study members’ scores were substantially lower than what we’d expect, indicating they were experiencing cognitive decline, even in middle age. 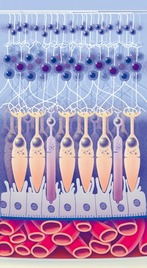 Why this matters While there are a number of potential causes of cognitive decline, papers from our research group are building up a picture of the factors associated with this outcome. We found people experiencing cognitive decline by 45 have older looking brains and more tiny bleeds and lesions, known as hyperintensities, in their white matter (measured using MRI). Our research found people with thinner retina had older looking brains and other structural brain abnormalities. This suggests cognitive decline, detected in its earliest stages, is associated with cell loss in the brain and retina. To investigate this question even further, we are now focusing on measuring study members’ levels of a specific type of protein (phosphorylated tau pTau181) which is abundant in neurons and deposited in cells in several neurodegenerative diseases. This is thought to be one of the earliest indicators of Alzheimer’s disease and it will help us to understand whether the changes we are observing are specific to Alzheimer’s disease and how early they can be detected.  Developing treatments for advanced stages of Alzheimer’s disease has been ineffective so far, and it seems likely future pharmaceutical treatments will be most effective in the earliest stages of the disease. Also lifestyle-based intervention may help to mitigate symptomatic cognitive decline. This makes early identification of people who would benefit from these interventions extremely important. Author: Ashleigh Barrett-Young Postdoctoral Fellow in Psychology, University of Otago This article is republished from The Conversation under a Creative Commons license. Read the original article here: theconversation.com/a-window-to-the-brain-the-retina-gives-away-signs-of-alzheimers-disease-and-could-help-with-early-detection-188655 Aged Care New Zealand Issue 02 2022 Suitable floors for aged care environments |
AuthorShonagh O'Hagan Archives
April 2024
|
























 RSS Feed
RSS Feed