 Leaky water works - Incontinence There are many myths about incontinence, which are not necessarily true. For instance many people believe incontinence is an inevitable consequence of ageing or if you drink less it will improve the problem. Neither of these beliefs is helpful. Some facts about our Water Works:
There are two types of incontinence – Stress and Urgency. Stress incontinence With stress incontinence there may be leaking when coughing, sneezing, jumping, lifting, pushing, laughing and pulling. This is caused by weak pelvic floor and urethra sphincter muscles. The trick is to strengthen your pelvic floor and urethral sphincter muscles and tighten your pelvic floor muscles before stressful activity occurs. Urgency incontinence Urgency incontinence is the sudden need to go, for example, when opening the front door you generally get the urge. It’s caused by an overactive bladder, which has been trained to empty before it’s full. Typically small amounts of urine are passed more frequently -10 plus times a day. Preventing or fixing incontinence
For both types of incontinence strengthening your pelvic floor and urethra sphincter are important. To do this:
Once you’ve mastered the pelvic floor exercises, practice regularly eg every time you stop at red lights. Tips for managing and training urgency incontinence When you experience the sudden urgency to pass urine, it is often associated with a feeling of panic. The following may help:
If desperate:
If you are still struggling there is help:
You don’t have to suffer alone - contact us we can help Ph: 03 3775280 Email: [email protected] Web: www.therapyprofessional.co.nz Reference: Women’s Waterworks – Curing Incontinence by Pauline E Chiarelli  Teaching Shaving Skills Shaving is a major part of growing up and for a boy, it signals the transition from childhood into manhood. Shaving is a complex task, which requires consideration of safety and sensory challenges. How can you make this easier? Get him used to the idea he will be shaving his face one day by:
We would recommend using an electric razor to start with, as they can be easier and safer to use. However, for some, the noise or vibration may be too much and a razor blade may more successful. Like all skills, there are a large number of smaller skills or activities used when shaving eg with an electric razor.
To assist teaching, take photos of each of these steps:
If it is not possible, try and locate pictures from the internet showing the shaving steps. Put the photos or simple pictures in the correct sequence with simple words describing the activity. Use this schedule as a prompt while teaching. Initially you may have to use verbal and physical prompts along with the schedule. If you are experiencing any problems with the development of these skills our Occupational Therapist may be able to help. Just contact us at Therapy Professionals Phone: 03 3775280 Email: [email protected] Web: therapyprofessionals.co.nz https://www.carautismroadmap.org/shaving-for-young-men/  About Dietitians Dietitians help you to improve your health, wellbeing and prevent illness through good nutrition. They can translate scientific information about nutrition into practical dietary advice and tailor an eating plan based on your individual factors (age, medical history etc). Dietitians can help with a range of health problems and chronic diseases such as:
They will recommend practical solutions for:
Dietitians are able to prescribe:
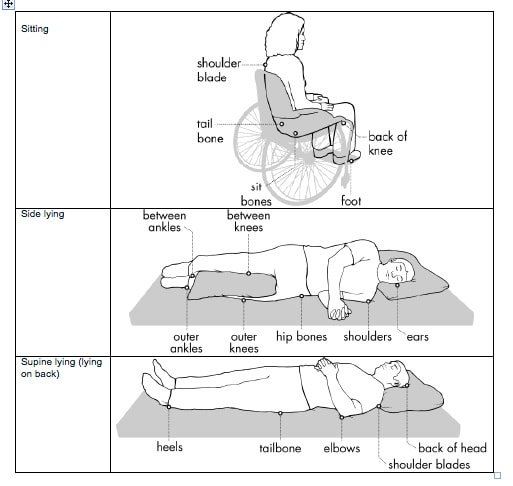
What's the difference between a Dietitian and Nutritionist? Dietitians are health professionals registered under theHealth Practitioners Competence Assurance act 2003 and meet standards required by the NZ Dietitians Board. Dietitianshave a science degree in human nutrition as well as a postgraduate Diploma or Masters in Dietetics. By law, a Dietitian must hold a NZ current practicing certificate, participate in a continuing competency programme and adhere to a code of ethics. Nutritionists: The term nutritionist is not protected and can therefore be used by anyone regardless of qualifications. Nutritionists who meet set criteria are able to become registered Nutritionists with the Nutrition Society of New Zealand. Therapy Professionals has a Dietetic service, so if you need help you just call us we come to you. Therapy Professionals Ltd Phone No: (03) 377 5280 Email: [email protected] Website: www.therapyprofessionals.co.nz Skin injuries caused by pressure For those of us caring for people who barely move or rely on others to move them, it is important to know how to best look after their skin. Pressure injuries, otherwise known as pressure areas, ulcers or bedsores, are among the negative effects of immobility. What is a pressure injury? A pressure injury is damage to an area of skin, usually around a bony part of the body, which has been under pressure for some time. The pressure stops the blood flow feeding the skin in the area and if the pressure is not removed the skin will break down and eventually become an ulcer. Friction from chaffing, or rubbing over these bony areas can also cause sores and ulcers. What areas are prone to pressure injuries? The diagrams below indicate where most pressure injuries generally occur, however people with unusual posture may develop them elsewhere. Who is likely to develop pressure?
Anyone who is immobile or can’t feel any sensations are at serious risk, especially those who:
How will I know someone is developing a pressure injury? The skin area around a bony part of the body may:
How can I prevent pressure injuries? A pressure injury is serious, can take a long time to heal, and many are preventable. We can help prevent pressure injuries by relieving direct pressure on the bony areas, taking good care of the skin and having a healthy diet and adequate fluids. Here are a few tips: Avoid direct pressure
Skincare
Diet
What should I do if you think a pressure injury is developing? Immediately reposition the person to completely take all pressure off the affected area and follow all the prevention tips above. Seek help from:
How can Therapy Professional’s Therapists can help? Our therapists can help with:
Dietitians: advise on:
Occupational Therapists: advise on:
Physiotherapists: advise on:
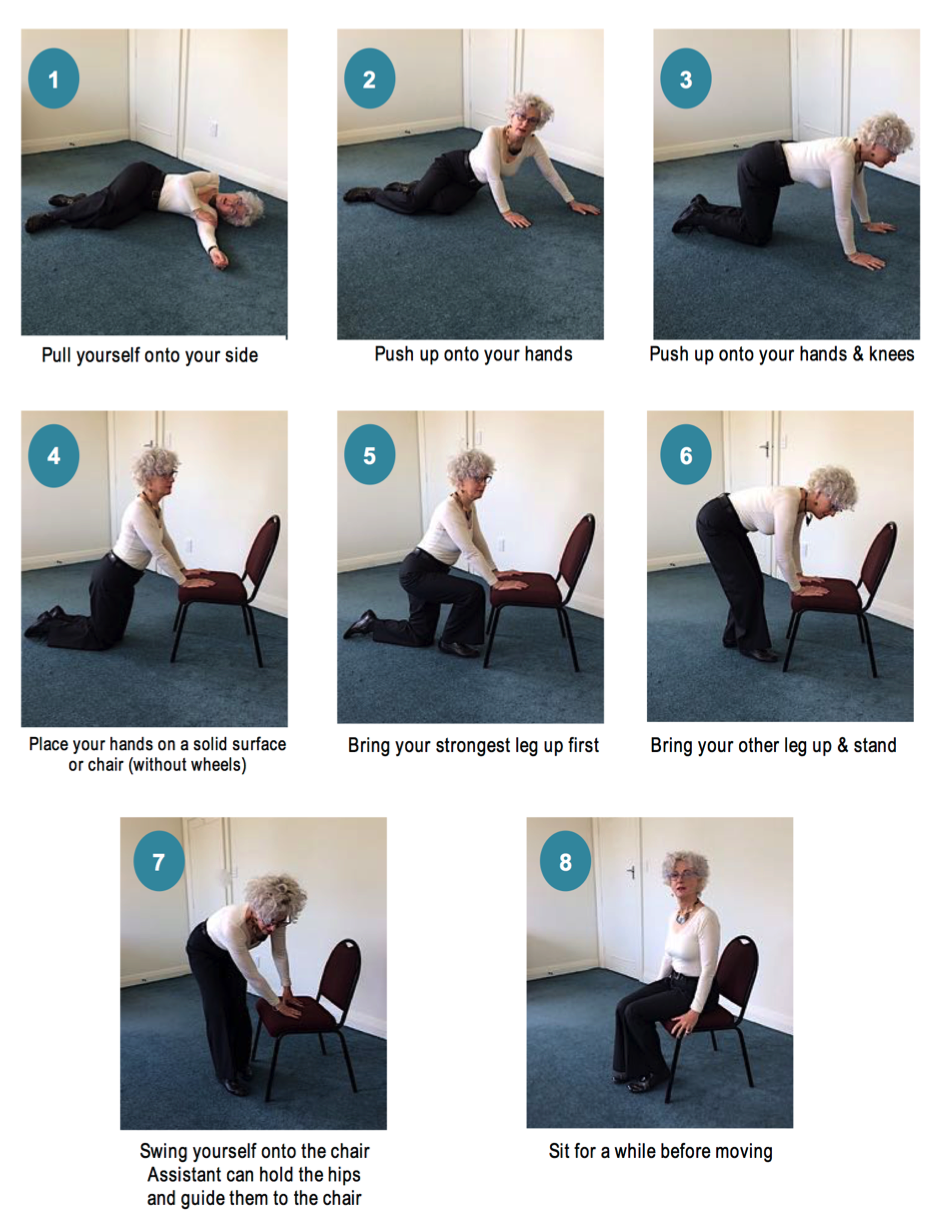
If you require education on prevention and management of pressure injuries, our friendly Physio and Occupational Therapists and Dietitians can help, just contact us at Therapy Professionals. Ph: 03 377 5280 Email: [email protected] Website: therapyprofessionals.co.nz Getting yourself up from the floor Currently, one in seven New Zealanders are 65 years and over. Around 30% to 60% of people in this age group have a fall each year. And 10% to 20% will end up in hospital with a fracture. Those over the age of 85 are 15 times more likely to fracture their hip in a fall than a 65-year-old. Hip fractures can have a huge impact, with 30% of those over 85 who suffer one, requiring placement in aged residential care. It’s important for those of us who are ageing and those around you, to know how to get up off the floor if you are not badly injured. The majority of calls to London ambulances from over 65 year olds are for help after a fall. Of these, 40% do not need hospitalisation – they simply cannot get up from the floor. Many carers hurt themselves, and the person they are trying to get up off the floor, because of lack of knowledge. To avoid further injury, here are some tips on how to get yourself or help someone up from the floor:
Follow the instructions in the Chart below: Our friendly Physiotherapists recommend all older people, their families and carers practise getting up from the floor regularly, before you need to do so, after a fall.
If you want advice on falls prevention our friendly Physiotherapists can help, just contact us here at .Therapy Professionals Ph: 03 377 5280 Email: [email protected] Website: www.therapyprofessionals.co.nz |
AuthorShonagh O'Hagan Archives
July 2024
|

 RSS Feed
RSS Feed