|
Exercise Beats Arthritis Therapy Professionals Ltd has a long tradition of helping people to maintain and improve their fitness. Their team of physiotherapists, occupational therapists, dietitians, music therapists and speech language therapists, all contribute their special skills to helping people increase their feeling of wellbeing. Arthritis is no longer just a disease of ageing. According to a new report commissioned by Arthritis New Zealand one in six people aged over 15 has arthritis and the figure is expected to increase by 2020. As specialists in physical exercises the physios recommend for people of all ages joints will benefit from exercise. Commonly asked questions are as follows: 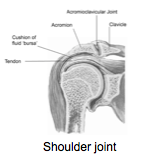 How does exercise help our joints? Exercise:
 When a joint is damaged or inflamed Rest it briefly, however we need to move the joint again as quickly as possible. Medication for pain relief or moving under water helps us keep moving the painful joint. What about the rest of your body? A painful or stiff joint, even a very small joint can upset your:
What exercises are right for you?  Exercises that put healthy stress on joints are:
(not swimming or cycling) 
and walking against a current in water, housework, gardening 
 Exercises for overall wellbeing:
Whatever you require, exercises need to be:
Pool: Pool exercises with water to help movement are useful.
for more information about their pool exercise programmes If you are struggling to exercise ,Therapy Professionals friendly physiotherapists are available to assess your needs and provide you with a personal exercise plan for your Arthritis. Just contact us: Phone: (03) 377 5280. Email: [email protected] Transdisciplinary Teamwork In 1987 Clare O’Hagan, the founder of Therapy Professionals Ltd attended the World Congress of Physical Therapy and heard a lecture by Carol Davis on Transdisciplinary Teamwork. From that moment Clare wanted to develop such a team. It wasn’t until 1997 when she got the opportunity. It was a slow process to start with as the disciplines were struggling to work in a multidisciplinary way. By the early 2000’s the team was humming and her dream was realised. Below is Carol Davis’s article on transdisciplinary teamwork. Philosophical Foundations of Interdisciplinarity in caring for the Elderly: or, the willingness to change your mind.
Carol M Davis, Ed. D Associate Professor Department of Physical Therapy, Sargent College, Boston University, Boston, MA 02215, USA. INTRODUCTION Medicine alone rarely, if ever, meets all of most patients’ needs. Other health professionals assume the responsibility of caring for patients’ multiple other needs with a common goal of the highest level of independent function, thus the greatest quality of life possible, for each person. When health professionals from many disciplines attempt to work together in caring for the elderly patient, the end product of this effort can have various characteristics. This paper examines the characteristics of various outcomes, and describes what factors enhance the process. Finally the suggestion is made that the processes of interdisciplinary or transdisciplinary result in the best possible outcome of care for the patient. THE CONTINUUM TOWARD TRANSDISCIPLINARITY Few health care professional students in the United States receive adequate training in learning how to work well with others for the good of patients. Indeed, young beginning practitioners often feel more than stressed in simply maintaining access to their own professional knowledge and skill. Learning to work with others takes place on a continuum of growth that can be described in the following model: Unidisciplinary Feeling confident and competent in one’s own discipline Intradisciplinary Believing that you and other fellow professionals in your own discipline can make an important contribution in care Multidisciplinary Recognising that other disciplines also have important contributions to make Interdisciplinary Willing and able to work with others in the joint evaluation, planning and care of the patient Transdisciplinary Making the commitment to teach and practice with other disciplines across traditional disciplinary boundaries for the benefit of the patient’s immediate needs. (United Cerebral Palsy 1) The increasing effectiveness of each of these processes can be illustrated with the help of the following case example. An 85-year-old patient is admitted to the geriatric evaluation unit with a cerebral vascular accident with right hemiplegia, hemianopsia, and aphasia. He is accompanied by his 78-year-old wife. They had been living together at home prior to his stroke one month ago. Since that time the patient was in the hospital for resolution of his acute problem, then transferred to a nursing home for careful nursing care until he stabilised. Mr Walker was a tailor and lives on a modest social security income. His wife receives no social security. Their finances are assisted by monthly cheques from their son who lives in another state 1000 miles away. Mr Walker is diabetic. Mrs Waker is quite well but very lonely without her husband of 60 years. They were active in the Methodist church but were driven to church each Sunday before Mr Walker’s stroke, as neither could drive any longer. Mr Walker’s physician illustrates unidisciplinarity and intradisciplinarity as he evaluates the patient upon admission to the hospital. He believes that his discipline of internal medicine is very suited to the care of this patient, but his area of expertise in gastrointestinal cancer restricts his confidence that he can uncover and treat Mr Walker’s circulatory problem to resolve it adequately. Thus, he requests his colleague in internal medicine who is a cardiac specialist to see the patient as well. Multidisciplinarity occurs as he writes the order for the patient to be seen by the physical therapist, occupational therapist, speech therapist, the psychologist, the social worker and the nutritionist. When this group of practitioners evaluate the patient and plan their care, all separate from each other, communicating only by way of the patient’s record, they are practicing multidisciplinarity. Just as in a ‘jar of jelly’ beans, the end product of care is no more than the sum total of all the parts. Patients complain about multidisciplinary care when they say, “I’m not answering that question one more time!”. Or, “I’ll only give blood once today – you people get together and figure out which one of you is going to stick me and when.” Practitioners complain about multidisciplinary care when the goal of the physical therapist to increase Mr Walker’s endurance in ambulation is thwarted by the nurse who ties him in bed so he cannot get up and walk around for he might fall. Interdisciplinarity can be recognised as superior to the aforementioned when it’s working well. In the Journal of Medicine and Philosophy Maurice de Wachter offers five steps to interdisciplinarity (De Wachter 2):
Thus, interdisciplinary process is composed of more than just several health professionals gathered around a table to discuss Mr Walker. Each sits down and, in essence, brackets his or her professional-discipline identity, places it to the side and assumes the new identity of “team member.” This act of bracketing is critical to the success of interdisciplinarity. Just as in algebra or language analysis, brackets serve the purpose of setting aside, without destroying, what is bracketed. In other words, identity as a physical therapist, for example, is available to me and, indeed, informs my contribution to the team, but I do not allow it to keep me from hearing the reports of other team members and helping to decide on a team goal and plan of care for this patient. In short, each of us sits down at the table and listens to the others with a willingness to allow others to change our minds. In this way the very best of all possible plans is agreed upon. Unlike the “jar of jelly beans”, the product of this effort is larger than the sum of all the parts. Indeed, ideally professional boundaries are transcended and flow into each other with ease, much like the colours of a rainbow. Finally, transdisciplinarity represents the highest progression in the process of patient care. Hospice care illustrates this process quite adequately. Health professionals teach each other, the patient and the patient’s family how to perform aspects of care reaching beyond professional boundaries with the immediate need of the patient being foremost. If the physical therapists arrives to work with a patient at home and learns she has not yet taken her pain medication, she doesn’t wait for the nurse to arrive to give it, nor the husband to make the toast to take with it. She does it herself. Likewise she teachers the nurse, husband and volunteers how to help the patient move about in bed and walk to the bathroom. Integrated, smooth, coordinated congruent care with the patient’s immediate needs at the centre of the effort marks transdisciplinary care. Individuals come together without territorial professional boundary needs to guide their role and responsibilities. This is what makes it the highest form of care. Transdisciplinary care is a mature and humble way of being in the world. Factors which interfere with interdisciplinary and transdisciplinary care include:
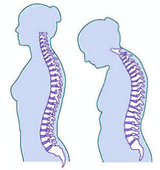
Factors that enhance interdisciplinarity and transdisciplinarity are the opposite of these limiting factors. Central to these two processes is a mature, secure, self-confident practitioner with excellent skills in communication and teaching who primarily values that the patient’s needs be met regardless of who meets them. The making of such persons takes time and commitment to the beauty and value of the rainbow. 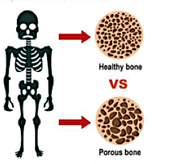 What is Osteoporosis? Osteoporosis is a condition in which the bones become fragile and break more easily. This is because calcium and bone tissue, the major building blocks of bone, are being lost. Bones are denser on the outside and have an open honeycomb structure on the inside. When calcium and bone tissue are lost, the outer shell becomes thin and the ‘honeycomb’ develops larger holes. This weakens the bone, which is then more likely to break. The process of bone loss begins from about the age of 35 onwards as part of the normal ageing process. Osteoporosis is very common and is a major cause of skeletal problems worldwide. About one third of women in Australia and New Zealand will suffer fractures by the time they reach their seventies. Osteoporosis is also found in men, but is much less common. How is Osteoporosis caused? There are different stages of bone changes throughout life. The first stage occurs up to the age of 35 when bone reaches its maximum strength. From 35 years of age onwards, there is a slow loss of bone strength in both sexes. In women the fall in oestrogen levels at menopause leads to loss of bone calcium and structure over several years. In younger women, oestrogen is important in preventing calcium being lost from the bones. How do you know if you have Osteoporosis? You often show no sign of osteoporosis until you have a fall and break a bone. Breaks are more common in the bones of the spine, the hip and the wrist. These breaks can occur even after a minor fall. In the spine osteoporotic fractures lead loss of height and acute episodes of back pain. These vertebral crush fractures give a forward tilt or bend to the spine producing the ‘Dowager’s hump’ appearance and preventing the maintenance of posture. Who is at risk of Osteoporosis? There are a number of factors that make you more likely to develop osteoporosis. Some of these factors you may be able to alter while others you cannot. You are more likely to develop osteoporosis if you:
 You are also at higher risk of osteoporosis if you:
However, these risk factors may not be a completely reliable guide to your individual risk of osteoporosis. Your bone density (but not bone structure) can be measured if you or your doctor is concerned about your risk.  What can you do to reduce the risk of Osteoporosis? The best way to prevent osteoporosis is to reduce your exposure to the risk factors mentioned. These include maintaining an adequate calcium intake, avoiding high intakes of alcohol and caffeine, and stopping smoking. Dairy foods, such as cheese, milk and yoghurt, are the best sources of calcium and you should aim for 3 serves daily. Each of the following is roughly equivalent to 1 serve: 1 (250 ml) glass of milk; a 200 g tub of yoghurt: or a 35 g piece of cheese. If you are experiencing or have just experienced the menopause, your doctor may decide to give you hormone replacement therapy. This replaces the oestrogen that your body no longer produces and helps prevent the loss of calcium from the bones. Weight bearing exercise such as walking, jogging, tennis, golf, dancing and bowls helps to maintain bone strength. What can be done to treat Osteoporosis? If you are in pain your doctor may prescribe pain relievers and muscle relaxants. Bed rest may be useful initially and a back brace may also be of help. Gentle exercise, such as walking, can help to improve bone strength. You may also be given medicine, which can help prevent bones losing their strength. These medicines include calcitriol, the active form of Vitamin D, anabolic steroids, hormone replacement therapists and calcium supplements. Please refer to your doctor if you have any further questions. Reference: Adis International, Roche If you need help to get mobile, exercise or you need dietary advice our friendly physiotherapists and dietitians can help just contact us.
Ph: (03) 377 5280 Email: [email protected]  Occupational Therapy Hip Care Tips - for six weeks after your operation Do not:
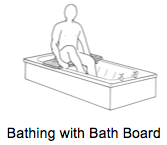 Bathing: Avoid sitting in the bath for the first six - eight weeks. If you do not have a shower we will order a bath board for you and you will be instructed how to get in and out of the bath.  Showering: We can arrange for you to have a high shower stool in order to take weight off the operated leg and to reduce the chance of falling  Dressing
 The Bed:
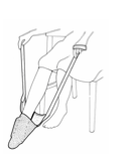
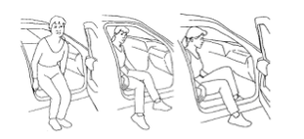 The Car Follow your surgeon’s advice about driving To get into a car put your bottom on the seat and swing your feet into the car. Stairs NB Good leg (leads) up to heaven. Bad leg (leads down) to hell. Sports/Hobbies Check with your surgeon before restarting active sports or hobbies ie cycling, gardening, bowls. Sexual Activity Ensure any sexual activity does not place any strain on your operated hip and that your hip doesn’t bend greater than 90º for at least three months post-operatively. Home Help If you require assistance with meal preparation and/or home help ask your hospital nurse. If you need advice on equipment contact us at Therapy Professionals as our friendly Occupational Therapist can help. Just contact us:
Phone: 03 377 5280 Email: [email protected] Website: www.therapyprofessionals.co.nz |
AuthorShonagh O'Hagan Archives
July 2024
|


 RSS Feed
RSS Feed