 Teaching Crossing the Road Skills For most adults, crossing the road is automatic behaviour, we do it without thinking and we don’t consider how complex a skill crossing the road is. Nor do we consider how our life might be curtailed if we couldn’t successfully negotiate our way around roads. Some of the skills required for crossing the road include:
In some cases even more advanced problem solving is required. For example, if the traffic light signals say it is safe to cross and a motorist continues through the intersection, we need to be able to identify the car is not stopping and decide to wait for it to pass before crossing. Traffic-related mishaps account for a large number of deaths and injuries amongst our society’s children and youth. For youngsters with special needs, the risks can increase dramatically due to: 
,Acquiring these skills is important for our independence and quality of life. For those of us with special needs, who struggle to learn road skills easily, this can be a big barrier to independence.
Parents, educators and support workers need to work much harder to teach young people with special needs about street and traffic safety and employ strategies to help compensate for the challenges they may face. The first step is to break the skill down into its separate skills and teach each of these skills step by step. If you are struggling to teach a young adult to cross the road and would like some help our friendly Occupational Therapists at Therapy Professionals Ltd can help.  Enable Equipment Service (Ministry of Health Funded Equipment Management Scheme) If you’re in need of equipment to assist you to function in life, you may be eligible for Enable equipment. The equipment is on loan from the Ministry of Health free of charge, however the assessment and application may cost you, so please discuss with a therapist. Therapy Professionals Ltd’s Physio and Occupational Therapists are accredited assessors for Enable equipment in the following areas: 1. Personal Care & Household Management a) Personal equipment to enable you to carry out personal care activities in their home, at work or place of study, such as: - eating and drinking - personal hygiene (washing and toileting) - getting dressed - transferring from the bed or chair - getting in or out of the home b) Household Management equipment to enable you to carry out essential household tasks to return to, or remain safely your home, such as the preparation of food and drinks, if you live alone or by yourself for much of the day.  2. Walking & Standing a) Walking equipment to support you with walking and transferring. b) Standing equipment to support you to maintain a good functional position and body alignment in standing. 3. Basic housing modification equipment to ensure your safety at home such as: - handrails, - wedge threshold ramps - lever taps or - internal door widening. 4. Complex Housing Modifications are where the alterations to the structure of the property are made. 5. Wheeled Mobility and Postural Management Level 1 and credential lying advice and recommendations related to wheeled mobility, seating and postural management. The Process: It takes between two hours and several months depending on the complexity and expense of the equipment. - an Enable accredited therapist assesses your need for equipment and if you’re eligible. - Therapist completes the Enable service request electronically if funding is ‘available’. While funding may be available, Enable has final discretion on eligibility for equipment. - Equipment is trialed or issued to you. - The therapist will follow up on the use and appropriateness of the equipment. Keeping Records of Equipment
Most equipment comes with an ASSET NUMBER. You or the residential providers are responsible for keeping records of asset numbers and maintenance of the equipment. The asset number stickers can fade and come off especially on soft fabrics, eg slings. We recommend you develop a system to record asset numbers permanently. (eg: taking a photo of the piece of equipment and asset number. Keep it somewhere safe or in your client’s file). Repairs and Maintenance: Contact one of the subcontractors listed below: More Mobility/ Mobytech Ltd 113 Blenheim Road, Christchurch 8041 Phone: (03) 348 3460 Option 3 or 027 516 2340 Email: [email protected] [email protected] Website: http://www.moremobility.co.nz Personal Mobility Systems (Wheelchair Services (SI) Ltd) (not generally a mobile service) 29 Shakespeare Road, Christchurch 8240 Phone: (03) 366 8815 or 0275 383 584, Free: 0508 662 454 Email: [email protected] Website www.mobilitysystems.co.nz Rehab Enterprises, mobile workshop. Contact Owen Henwood on phone: 027 230 5974 or email: [email protected] Alteration or Modification of Equipment If you wish to have equipment altered or modified this is not a repair or maintenance. Call the therapist. Equipment no longer needed for clients: Ring Enable and ask for it to be picked up Phone: 0800 171 995 OR Residential providers - If another client would benefit from the equipment, call the therapist, they will assess and if suitable re-issue the equipment. 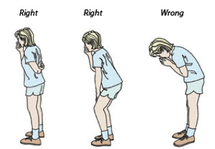 Eating and Drinking Problems related to Dementia A number of eating and drinking issues may occur for those with dementia including under or over eating and swallowing problems. Swallowing difficulties (dysphagia) related to dementia and Alzheimer’s have increased with longer life expectancy. The prevalence among those individuals with intellectual disability is also increasing, however at a younger age as they prematurely age. Swallowing difficulties: How do you know someone has an eating and drinking difficulty? They will have some or all of the following signs while or after eating and drinking:
 Under-eating As we age our appetite decreases. For those with dementia this decrease in appetite can be more pronounced. In the early stages under-eating can be prompted by depression and later on due to forgetting to eat or even how to eat. Medications can affect appetite too. Suggested support
Over-eating: For some people with dementia an increase in weight can be an issue for a number of reasons. They:
 General suggestions:
Equipment:
 Use visual and other strategies:
Safety:
The role of the team and when to refer:
If you need help with someone with a swallowing problem, just contact us at Therapy Professionals Ltd, our friendly Speech Language Therapist can help.
Phone: 03 377 5280 Email: [email protected] Website: therapyprofessionals.co.nz  THE LUNCH BOX DILEMMA Making school lunches can be a great source of stress for many parents, myself included. We can fall into the trap of giving our children exactly the same lunch day after day and wonder why they stop eating them! Or we go for the convenient packs of chips, dairy foods and muesli bars, which often children love, however they are not a healthy option. When you’re tired and busy it’s hard to take the time and have the imagination to produce good healthy lunches for your children. A few years ago one of our Dietitians, a parent of two young boys, put together these guidelines to help we parents who are struggling to put lunch boxes together. How to put together a tasty and nutritious lunch box.
Choose from these foods to get the balance right. 1) Wholegrain bread, wraps, pita bread, roti, rolls, rice, noodles (not 2 minute noodles), pasta, rice wafers etc. COMBINE WITH 2) Chicken, shaved ham, lean meat, fish/tuna, eggs, cheese, peas/beans/lentils, hummus, nut butters and hard boiled eggs and nuts etc ADD 3) Whole or cut-up fruit, berries, grapes, pottle of stewed/tinned fruit, salad, vege sticks, cherry tomatoes etc. Fruit and vegetables provide essential vitamins and fibre for good health and digestion 4) Include healthy fats for taste and brainpower such as avocado, salmon or oily white fish (tinned is fine) and nuts. OPTIONAL EXTRAS 5) Dried fruit, popcorn, pikelet, small homemade muffin, or plain biscuits, bite-sized cereal eg Weetbix Bites/Miniwheats, small can creamed rice, nuts (if allowed), crackers, corn thins, low sugar yoghurts or natural yoghurt with frozen berries. Makes lunch boxes appealing and provide energy 6) Fluid – Water is the best choice; the good thing is it’s free from any drinking fountain and tap at school. If you need more help putting lunch boxes together for you children, especially if you have a child with a health condition or disability, our friendly Dietitians can help, just contact us at Therapy Professionals Phone: 03 3775280 Email: [email protected] Written by Helen Gunn, Mother of two and Dietitian for Therapy Professionals Ltd Ph. (03) 377 5280 |
AuthorShonagh O'Hagan Archives
July 2024
|

 RSS Feed
RSS Feed