|
Seating Advice for Residential Care The frail elderly and disabled in care spend much of their day sitting, often in unsuitable chairs, which restrict their mobility and cause them to adopt slumped postures. Correct seating allows clients to:
When a resident has difficulty rising from an armchair, consider the seat height, depth, width, slope and firmness, and the armrest height. When choosing an armchair for your residents consider these things:  a) Height: For comfort and ease of getting out of the chair:
b) Width: There needs to be a space of 2-3 fingers either side of the body to allow wriggle room and to keep the armrests comfortable. c) Depth: The depth needs to ensure a good upright posture and for ease
 d) Back rest needs to:
e) Arm rests need to:
Residents come in all shapes and sizes, we recommend Residential Providers
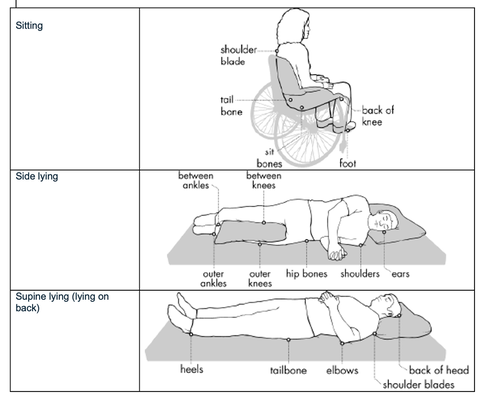
Choosing wheeled chairs For staff safety when choosing wheeled chairs, ensure the wheels are larger enough to push easily on all floor surfaces while allowing the ambulant person’s feet to rest on the floor so they can stand easily. If your current wheeled chairs are hard for staff to push, see if you can get larger castors or wheels, or check that fluff is not restricting the wheels.. Couches We don’t recommend couches as they are harder to get out of and harder to assist someone to stand. Skin injuries caused by pressure |
AuthorShonagh O'Hagan Archives
July 2024
|






 RSS Feed
RSS Feed