 Choosing a Comfy Armchair Ageing bodies change shape and our favourite seats may not be suitable anymore. Believe it or not, having the right armchair may make the difference between staying independent or not! If you find it hard to get out of a chair once in it, you're less inclined to get out of it, until you have to. Getting in and out of chairs helps keep our legs strong, assists us to keep our sense of balance and encourages exercise, which is good for most of our bodily functions. When choosing an armchair consider these things: a) Height: For comfort and ease of getting out of the chair:
b) Width: There needs to be a space of 2-3 fingers either side of the body to allow wriggle room and to keep the armrests are comfortable. c) Depth: The depth needs to ensure a good upright posture and for ease of getting out of. The:
d) Backrest: Needs to:
e) Armrests: Need to:
f) The chair surface: Needs to:
It’s important to have the main user sit in the chairs for some time and get out of it a number of times before deciding which to purchase. If you need any advice on purchasing a suitable chair our friendly physios and occupational therapists can help, contact us as follows: Ph: 03 377 5280 Email: [email protected] Website: www.therapyprofessionals.co.nz  Hearing Loss Causes Communication Breakdown At any age hearing loss negatively effects communication. During early childhood hearing loss, if not picked up, can delay children’s speech and language development significantly. Often poor speech clarity or language development is the first thing parents will notice. However if parents and others around young children can watch for the following milestones they may pick up a hearing problem early and be able to act quickly. Expected Milestones for babies 3 months
6 months
9 months
12 months
18 months
24 months
If you notice any of these milestones are not being met see your doctor and get your child’s ears tested. In older children it is more difficult to identify hearing loss because their speech skills are already developed. Nevertheless, these guidelines may help detect a possible hearing loss. The child:
You just have a feeling, but you can't put your finger on what your concern is. Don't let that stop you. Ask your doctor for a referral to ease your mind. Hearing loss can occur throughout adulthood with one in two adults over 65 years experiencing hearing loss, particularly with higher pitched sounds. Hearing loss causes frustration and communication problems regardless of age. If you think someone is deaf around you ensure they get their hearing checked regularly, there is likely to be a solution to either solve or reduce the impact of their hearing loss. Some guidelines on speaking to someone who’s deaf
Therapy Professionals Ltd Phone No: (03) 377 5280 Email: [email protected] Website: www.therapyprofessionals.co.nz  Do you have a Dry or Burning Mouth? A dry mouth happens because you’re not producing enough saliva and it can cause bad breath, a dry throat and cracked lips. Saliva is important for your digestion, protecting your mouth and teeth from decay and gum disease. In itself, it’s not a serious condition, however can be a symptom of another health condition, so tell your doctor. What causes dry mouth?
If you have a dry or burning mouth, firstly make sure you are drinking enough fluids - 6-8 cups a day is recommended. If you are drinking enough try the following:
If, after trying these things, you still have a dry mouth ask your Doctor or Dentist. Oil emulsion recipe Make up your own with grape seed or coconut oil. Use one tablespoon of oil to one tablespoon of water and swish around in your mouth. Baking soda mouthwash recipe
This mouthwash can be used for up to 24 hours, then discard. Swish the mixture around your mouth for about 30 seconds, then rinse your mouth with water. This is also a good mouthwash to use if you have sore gums, or other mouth injuries, since baking soda and salt have both been proven to speed healing. For more advice our friendly Dietitian can help. Just contact us at Therapy Professionals Ltd Phone: 03 3775280 Email: [email protected] Website: therapyprofessionals.co.nz  To Exercise or Not to Exercise? That is the question Here are a few tips to help you decide. You have got a fever:
You’ve got a cold
You’ve got the flu
You’ve had a recent asthma flare up or chest infection
You’ve had a bad night and feel too tired
Your muscles are sore
You’ve had a rough week
Don’t rush your comeback
If you need any advice on what’s the best sort of exercise for you we can help. Just contact us on Ph: (03) 377 5280 Email: [email protected]  ‘Young at heart, slightly older in other places’– eating and drinking problems and ageing. Swallowing difficulties (Dysphagia) are a common consequence of many health conditions, and head and neck surgeries, however swallowing difficulties can also be associated with ageing. Estimates suggest up to 20% of all adults over 50 may be affected. Changes might include such things as reduction in muscle strength for chewing, taste and smell, dental issues, dry mouth or throat, or recurrent illness such as pneumonia. These changes may result in poor nutrition/hydration, unintended weight loss, avoidance of eating in public, loss of enjoyment in previously enjoyed food, and/or a risk of food/fluid entering the lungs (aspiration) leading to pneumonia and chronic lung disease.  What might you notice?
Suggestions to help:
Who can you talk to?
Phone (03) 3775280, Email: [email protected] Website: http://www.therapyprofessionals.co.nz Our Dietitian or Speech Language Therapist will be happy to help.  The Magic Power of Diaphragmatic Breathing Breathing happens automatically like other bodily functions, such as:
These functions are controlled by our autonomic nervous system, which has two parts. The sympathetic system, which usually gets these functions going and the parasympathetic system, which stops them from happening. The sympathetic controls our fight-or-flight response, while the parasympathetic is in charge of everyday processes. Even though these functions are automatic, we can help regulate our automatic nervous system, with diaphragmatic breathing. This has many benefits — your heart rate and blood pressure can be reduced, helping you to relax. This all helps decrease the amount of stress hormone, cortisol, released into your body. Diaphragmatic or tummy breathing also helps:
Many of us breathe only using our upper chest cavity and when we are asked to breathe deeply we pull our shoulders up and expand the upper part of our chests. Breathing in this way does not make use of the lower capacity of the lungs. Diaphragmatic or deep tummy breathing is named after the diaphragm muscle. This muscle pulls air down into the lungs (like bellows) and as it relaxes, it rises up and forces air out of the lungs. 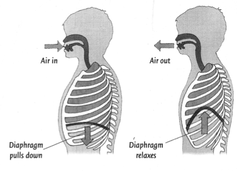 Learning to do diaphragmatic or tummy breathing takes time and conscious effort. Here are some instructions:
 Disability - A Family Burden We hear stories of families who never get a day off, elderly parents who are still looking after their disabled adult children, and children with less obvious disabilities not receiving any support. Often families with disabled members feel isolated, alone and are unaware of the help they can receive. This is especially true for those with the least obvious disabilities. Compounding the problem health professionals are often unaware of the range of help available or assume families are linked into the services they require. The trouble is the system for receiving government-funded supports is across a number of government ministries – Health, Education, and Welfare. These systems are hard to navigate, especially for stressed families and they don’t dovetail together easily. Also in the past 30 years government funded disability support services have focused on providing for a small group with the highest needs. No one would deny this group needs support, however this has left a large group who have been forgotten, many of whom would have benefited greatly from some assistance early in life, making them more independent and improving the quality of family life. There is help. If your child has not been in contact with the CDHB services, the best place to start is the Needs Assessment and Coordination service (NASC), a Ministry of Health (MOH) funded service. You can refer yourself or a family member without having to go to a doctor. This will give you access to a number of MOH funded and community services. The Ministry of Social Development has a range of benefits you may be able to access for yourself or a disabled family member. The Ministry of Education Special Education Services can be accessed for those at school. For your school aged child with special needs, it’s important to investigate the Ongoing Resources Scheme (ORS) and High Medical Needs Ministry of Education Funds as early as possible in their schooling. The sooner your child gets help the better. On the link below there are some handy links to government agencies, which may help relieve the burden of disability. There are many more organisations that can help, most of which are government funded. All the best navigating through this maze.  |
AuthorShonagh O'Hagan Archives
July 2024
|


 RSS Feed
RSS Feed