 Fatigue - An overview What is Fatigue? Fatigue is an overwhelming sense of physical or mental tiredness that may affect any or all areas of functioning: physical, cognitive, and social. For people who have had a brain injury, fatigue is a very common and persistent problem. ‘Mental’ versus ‘physical’ fatigue Physical fatigue refers to the fatigue that results from any kind of physical labour such as exercising, mowing the lawn, and playing outside with the children. Just after a brain injury, physical fatigue may be a problem. For example, it requires a lot of energy to relearn how to walk. For most people, physical fatigue tends to subside after about six months following the injury. Mental fatigue refers to the fatigue that results from ‘brain work’, such as working on the computer, writing a letter, reading the newspaper, conversing, studying, planning and problem solving, and driving. Although mental fatigue also decreases over time, it tends to be a very persistent problem that needs to be managed carefully. For most people it does not go away completely. Why is mental fatigue a common symptom of brain injury? It is not known exactly why fatigue is such a common problem for people who have had a brain injury. However, it is thought that fatigue results because the brain has to work a lot harder than it did prior to the injury. Some of the brain cells are damaged, and do not work as efficiently as they should – information does not flow as easily around the brain. The brain has to work harder to cope with this, resulting in fatigue. Also, the brain takes longer to restore its energy, meaning that it takes longer to recover from fatigue than it did prior to the injury. Fatigue may also be a side effect of some medication. Mental fatigue can affect the success of all rehabilitation efforts. Fatigue decreases concentration, memory, and social interactions. It increases irritability, distractibility, depression, and anxiety. Fatigue can cause confusion and decrease the ability to make good decisions. It may also increase physical symptoms such as headaches and dizziness. It is therefore very important to manage fatigue. What can be done about it? It is a good idea to slowly build up active hours, gradually increasing stamina. The number of home and social activities undertaken may also need to be reduced. There are a number of basic strategies that can be used to manage fatigue: 
‘Rest’ can be simply lying down, or sitting quietly. It does not have to be a ‘sleep’.
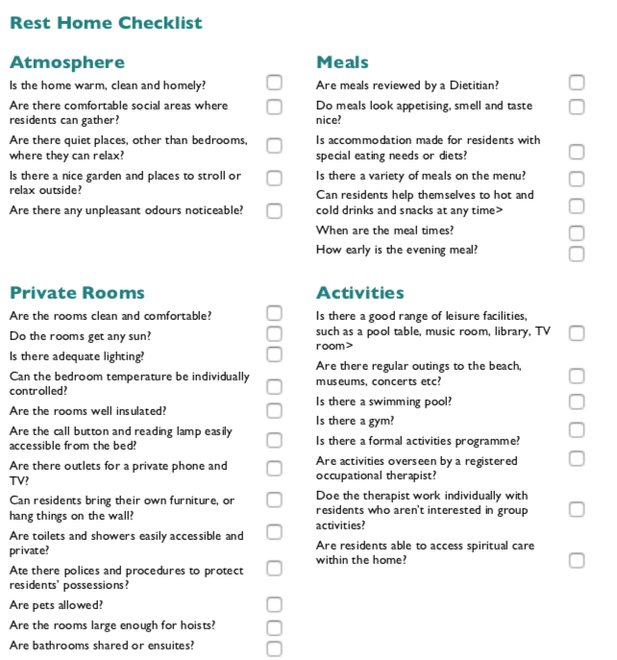
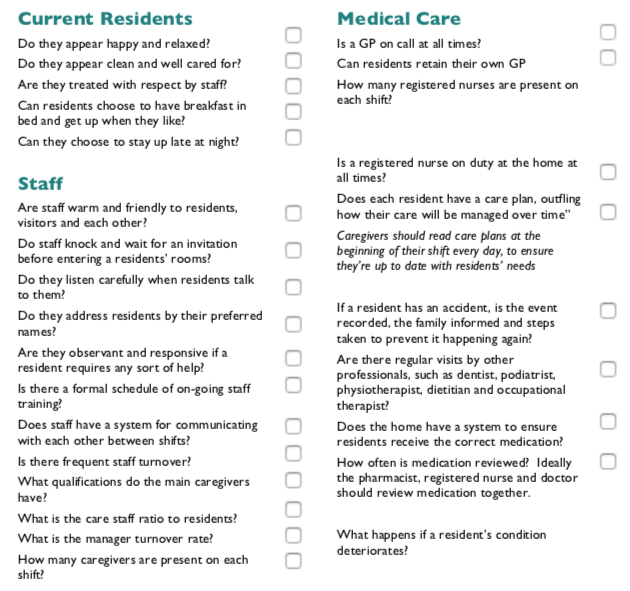
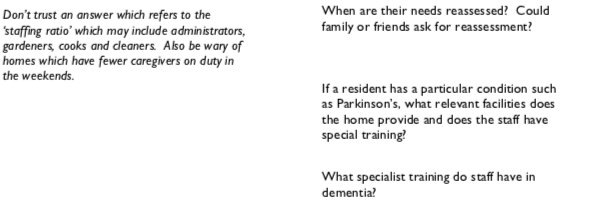
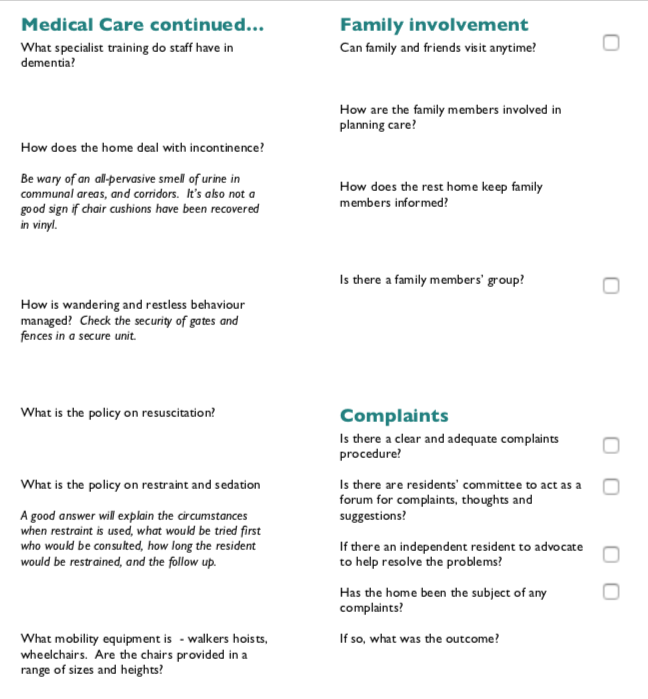
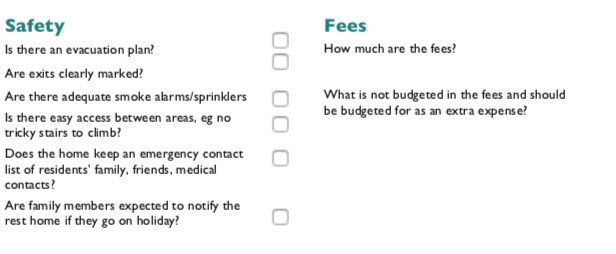
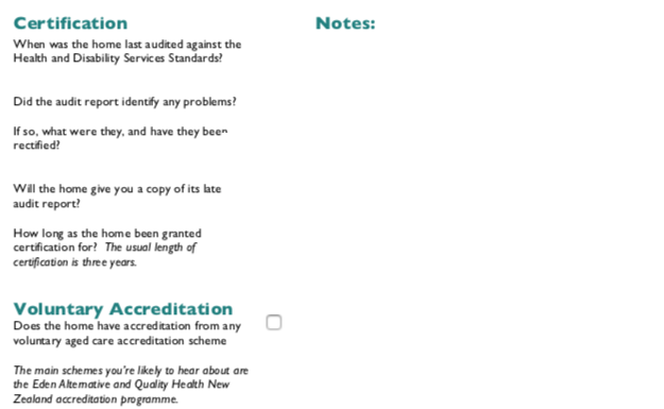
Conclusion Fatigue is a common and persistent problem following a brain injury, which may require some lifestyle changes. However, effective fatigue management can be achieved. Much of this revolves around weekly scheduling of activities, rest periods, and appointments. If you need help relaxing, with physical exercise or diet, our friendly therapists can help, just contact Therapy Professionals Ltd  Your Parents need Residential Care Therapy Professionals has work in Aged Care since 1985 and we have seen the industry grow and develop from almost a cottage industry to the corporate dominated industry it is today. We have personally experienced and watched others struggle to navigate their way through the whole process of entry into residential care. We know how hard it can be for you and your parents to accept it’s time for residential care (rest home, hospital, dementia and special care hospitals). Once this decision has been made knowing how to access care is not always straight forward. This information from the Ministry of Health can be very helpful when negotiating your way through the process. This link will take you to the following questions and answers on the MOH website. https://www.health.govt.nz/our-work/life-stages/health-older-people/long-term-residential-care/residential-care-questions-and-answers What is residential care? Is there a list of residential care providers? Who is responsible for funding residential care services for older people? What are the criteria for entry into residential care? How does a person apply for residential care? How does a person apply for a residential-care subsidy? What happens if the circumstances of the person in long-term residential care change? While the person is in care, what individual services/items do they have to pay for that are not covered by Government funding (the residential care subsidy)? What is a License to Occupy? If a person is admitted to hospital whilst in a residential care facility, do they have to continue paying for their bed at the facility? How does a resident make a complaint? Once you have the residential subsidy or have freed up the funds to enter residential care, you then have to choose which facility will suit your parent/s and you. Working this out will be limited by the availability of beds. At the time residential care is needed your preferred option may not be available. When looking at the options you need to have some way of comparing them. Consumer did a Rest Homes Checklist a number of years ago witch we have added a few items to. You may find this helpful. https://d3c7odttnp7a2d.cloudfront.net/assets/8159/Rest_Homes_checklist.pdf If you have an elderly family member struggling at home or in care and you want additional rehabilitation, just contact us at
Phone: 03 377 5280 Email: [email protected] Dyspraxia - what is it? Definition Dyspraxia is a brain-based motor disorder. It affects fine and gross motor skills, motor planning, and coordination. It’s not related to intelligence, but it can sometimes affect cognitive skills. Dyspraxia is sometimes used interchangeably with developmental coordination disorder. While some doctors may consider these separate conditions, due to a lack of formal definition, others consider them the same. Children born with dyspraxia may be late to reach developmental milestones. They also have trouble with balance and coordination. Into adolescence and adulthood, symptoms of dyspraxia can lead to learning difficulties and low self-esteem. Dyspraxia is a lifelong condition. There’s currently no cure, but there are therapies that can help you effectively manage the disorder.  Dyspraxia symptoms in children If your baby has dyspraxia, you might notice delayed milestones such as lifting the head, rolling over, and sitting up, though children with this condition may eventually reach early milestones on time. Other signs and symptoms can include:
As your child grows, you might also observe delays in:
 Dyspraxia makes it hard to organise physical movements. For example, a child might want to walk across the living room carrying their schoolbooks, but they can’t manage to do it without tripping, bumping into something, or dropping the books. Other signs and symptoms may include:
Although intelligence isn’t affected, dyspraxia can make it harder to learn and socialise due to:
Dyspraxia is different for everyone. There are a variety of potential symptoms and they can change over time. These may include: · abnormal posture · balance and movement issues, or gait abnormalities · poor hand-eye coordination · fatigue · trouble learning new skills · organisation and planning problems · difficulty writing or using a keyboard · having a hard time with grooming and household chores · social awkwardness or lack of confidence Dyspraxia has nothing to do with intelligence. If you have dyspraxia, you may be stronger in areas such as creativity, motivation, and determination. Each person’s symptoms are different. If you have a child with dyspraxia and you want help, our friendly therapists can help, just contact us on: Phone: 03 377 5280 Email: [email protected] Reference Healthline https://www.healthline.com/health/dyspraxia#adult-symptoms What is a Stroke? What you need to know (a great resource from the Stroke Foundation https://www.stroke.org.nz/what-stroke) A stroke is a brain attack. It is very serious, but many people go on to recover and live healthy lives. A stroke happens when a blockage such as a clot blocks the blood flow to the brain, or when a burst blood vessel bleeds into the brain. Over 11,000 strokes are experienced each year – that’s one every 45 minutes. Stroke is New Zealand's second single biggest killer and the leading cause of serious adult disability. But many New Zealanders who have a stroke recover and lead successful, happy lives. A stroke is a brain attack A stroke is a sudden interruption of blood flow to part of the brain causing it to stop working and eventually damaging brain cells. During a stroke, the cells in the affected part of the brain start to die and that part of the brain cannot work properly. This can affect a person’s ability to walk, talk, eat, see, read, socialise or do things they were able to do before the stroke. Many people with stroke may also have fatigue or problems with remembering, understanding or thinking properly. This short video is an excellent explanation of what a stroke is (courtesy of HealthSketch). https://www.youtube.com/watch?v=ryIGnzodxDs&t=2s 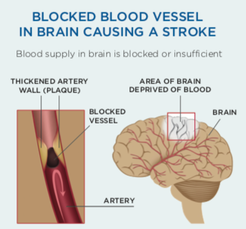 Types of stroke Ischaemic stroke: This is the most common type of stroke, particularly in older people. An ischaemic stroke occurs when a clot blocks an artery in the brain. The clot usually forms in a small blood vessel inside the brain that has become narrowed through high blood pressure, high cholesterol, diabetes or smoking. Embolic stroke: This occurs when a blood clot or piece of plaque (cholesterol or calcium deposits) on the wall of an artery breaks loose and travels to the brain. When this happens, the flow of oxygen-rich blood to the brain is blocked and tissue is damaged or dies. 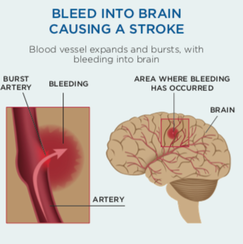 Haemorrhagic stroke: This occurs when an artery in the brain ruptures (bursts) and leaks blood into the brain (cerebral haemorrhage). This break in the blood pipeline means parts of the brain are deprived of blood and a stroke occurs. Blood irritates brain tissue, causing swelling and pressure, which cause further damage and loss of function. Subarachnoid haemorrhage (SAH) is when blood leaks into the surface of the brain. Intracranial haemorrhage (ICH) is when there is bleeding into the brain tissue itself. The impact of Stroke Different parts of the brain control a person’s movements, senses, emotions and intellectual functions. The effects of stroke depend on which part of the brain is damaged and how severe the damage is. Disabilities from stroke range from slight to severe. Some people make a speedy recovery and return to their normal lives. Others have disabilities that may improve with time and can be managed. For many, disabilities may last a lifetime. A small number of people will need full time medical care. Who does stroke affect? Stroke can affect people at any age. Although strokes often happen to older people, 25–30% of strokes are experienced by people under the age of 65 years. Stroke is largely preventable, yet each year about 11,000 strokes are experienced in this country. This number could be reduced by three quarters if all the recommended actions to reduce stroke risks were taken in the community. There is a list of facts and FAQs about stroke and treatment https://www.stroke.org.nz/facts-and-faqs The Stroke Foundation’s Life After Stroke section also takes you through treatment, rehabilitation, and what to expect after a stroke - we strongly recommend this free resource. If you have a relative who has had a stroke and you want additional rehabilitation or some support to improve life for you and them, our friendly therapists can help. Contact Email: [email protected] Phone: 03 377 5280 References
1 NZIER research report 2020: https://nzier.org.nz/static/media/filer_public/b4/6f/b46f7e92-be19-477d-b23c-7ba042d7cccd/social_and_economic_costs_of_stroke_-_2020_update.pdf 2 Ministry of Health (2018). Mortality and Demographic Data 2015, retrieved 14th August, 2018, from https://www.health.govt.nz/publication/mortality-2015-data-tables. 3 NZIER research report 2020: https://nzier.org.nz/static/media/filer_public/b4/6f/b46f7e92-be19-477d-b23c-7ba042d7cccd/social_and_economic_costs_of_stroke_-_2020_update.pdf |
AuthorShonagh O'Hagan Archives
July 2024
|

 RSS Feed
RSS Feed