|
Oral Care For those without teeth or are tube fed  Many people mistakenly think because they or the people they are caring for have no teeth or are fed via tube, there is no need to clean their mouths. This is simply not true. Oral and dental diseases can be a contributing factor to pneumonia as the levels of bacteria in the mouth and saliva are increased. If saliva or food/fluid contains these bacteria and enters the lungs (aspiration), it can increase the risk and severity of chest infections. If oral care is not maintained oral and dental disease is more likely and so are chest infections including pneumonia. Is oral care for everyone? Yes. Each individual should have a plan for oral care including anyone without teeth and even those who do not eat/drink orally (ie are tube fed). Why is oral care important?
How often?
Equipment that can assist with oral care:
How to do oral care/tips: Sometimes it can be hard to remember to do oral cares
If you are having any trouble implementing oral care, please don’t hesitate to seek help either from an oral hygienist, dentist or our friendly Speech Language Therapists. For advice especially for those with disabilities talk to our friendly Speech Language Therapists who are experienced with disabilities. Just contact us at Therapy Professionals
Phone: 03 3775280 Email: [email protected] Website: www.therapyprofessionals.co.nz Home away from home While many seniors like to be independent, they need thoughtfully designed spaces to be able to live in comfort and safety? from Aged Care New Zealand Issue 2 2021  Creativity can be put to the test when decorating a space for senior citizens. Whether it’s a single room, studio apartment, patio home or other living quarters, senior citizens have particular needs regarding their décor. While aesthetics and comfort are important, safety is paramount. A proper room layout and furniture arrangement is crucial to a senior’s wellbeing. Most nursing home rooms are modestly sized and bringing in too many personal items can make the room cluttered and dangerous. Keep walkways wide and clear to allow ample room for walking. Older people confined to a wheelchair or those that need the assistance of a walker or cane require even broader passageways. A single-level residence on the ground floor offers an optimal abode for seniors who have difficulty climbing steps. Even a single step that transitions from a kitchen to a sunken living area can be problematic for the elderly. Install a handrail on each side of the step as a reminder that it’s there as well as to aid for going up and down it. If it is a skilled nursing facility, then there may be a certain amount of medical equipment in place. When decorating, one can’t simply take it out because it is ugly. You also shouldn’t attempt to hide it behind other objects, as staff may need to access it quickly in an emergency. You may not be able to move furniture either. It is placed so that there is access to the appropriate outlets. What you can do, is take advantage of spaces that already exist, such as the bed, walls, furniture and windows. You can customise the décor to suit the individual’s personality and interests just by adding a few special touches. If it is a shared room, then the other’s privacy and territory must be respected too. One person’s possessions shouldn’t trickle over into the other side of the room, their lamps shouldn’t be pointed at the other person’s bed or reading chair, and one should make sure that any items that might be offensive or disturbing to the roommate are placed so they are not easily visible from their side. Shared rooms mean less space on either side of the divider too, so you will want to limit items that take up floor space, as well as things that are in ‘elbow space’ (tabletops) that they may need for other purposes, such as eating, writing, or working puzzles.  Safety Decorating a senior citizen’s residence with safety features should top the design list. Many older people don’t move around as well as they did in their younger years. Remove scatter and area rugs from the floors. Safety and ease of maintenance should be important considerations when choosing the right flooring for the elderly. For elders with an unsteady gait, a non-slip surface is a must.
The colour of the flooring tile is also an important consideration. Whites and light colours so not show up water spills, and even a little water on the floor can cause a nasty accident. Sofas and chairs that aren’t too low, deep or plush makes it easier for seniors to sit down and get up. In addition make sure the seating has stable arms that are tall enough for them to grab onto. A reclining chair supplies a comfortable seat that an elderly person can adjust to her own personal preferences. Substitute an upholstered ottoman for a traditional coffee table. An ottoman has no sharp edges or corners to scrape bare legs or bang your shins on and they are great for storing knitting supplies, magazines, a spare blanket and other odds and ends of clutter that make the room feel too claustrophobic. A bed with comfort level controls allows an older couple to adjust each side of the bed to suit individual needs, such as mattress firmness and reclining positions. All items inside the wardrobe should be easily accessible; a pulldown wardrobe lift is a useful accessory if rods are too high to reach. Decorate with dining, bedside and accent tables that have rounded corners for increased safety against sharp corners. Just aim for sleek designs that will fit well into any space and are easy to clean. Soft, woven furniture throws, lumbar pillows and dimmer switches add comfort to a senior’s home. Aesthetics Aesthetics plays a significant role in making an older person’s residence feel homey. If possible, paint the walls a warm but neutral colour – warm beige, sage green, creamy caramel – to generate a soothing ambiance. The wall colour should be a distinctly different hue than the floors so that seniors with weakening vision can readily discriminate between the two. The same principle applies to bedding; purchase contrasting bottom and top sheets for ease in differentiating between them. Senior citizens have often collected a ton of decorative items throughout their lifetime, which can quickly lead to a cluttered environment. Display only a few favourite articles on wall shelves and group small collectibles together for display in a lighted curio cabinet. Rather than putting all the favourite photos and knickknacks in a room at once, use very few at a time, then switch them around every so often to help the room look fresh and new. This is an especially good way to celebrate the changes of seasons. Health A very real consideration in an aged care environment is hygiene. If the person has any type of respiratory or contagious illness or infection, then you want to make sure all surfaces are something that can be wiped easily with a sanitising agent. This is not the best time to decorate with ornate scroll work that takes too much time to clean. Nooks, crannies, porous surfaces and linens that can’t be washed in hot water may harbour dangerous bacteria and re-infect or cause illness to others. Where, dementia is a factor, one may need to avoid overloading the room, since this can add to confusion. Busy prints are not a good idea, as they can appear to ‘crawl’. Choose furniture and storage containers that can be labelled, since photo labels can sometimes help the individual find items they need or want.  Lighting As we age, our eyesight deteriorates. Lighting should be cool and bright, and white light is preferred over yellow light. Plan to add adequate ambient lighting for safe navigation around the house, and task lighting for reading books or other hobbies.
Open up the views
As many elderly people are restricted to a room or the indoors, large windows or balconies are a lovely way for them to keep in touch with the outdoors. They should be able to get street views and views of the garden as much as possible. Windows should only have light shades so they get their daily dose of Vitamin D without needing to get outside. To sum up, it’s important to ensure that our senior citizens can live individualised spaces with a high degree of independence and dignity. It can also serve as a reminder to them, as well as to visitors, that they are more than just another resident. They are individuals with their own ideas and likes. Are your shoes safe? As we age our risk of falls increases. When we do fall, we are:
Making us more likely to fall again. There are many reasons falling occurs with ageing, it may be because of:
Falls are preventable. One of the many ways in which you can reduce your risk of falling is by changing the types of shoes you wear. Please take a few minutes to complete this checklist. It outlines characteristics of shoes that make them safer. Do your shoes fit well? Yes No (Shoes that are too tight or too loose can be dangerous) Do you mostly wear flat shoes? Yes No (High heels can be very dangerous) Does the sole of your shoe bend at the ball of your Yes No foot, not at the arch? (This is better for walking on uneven surfaces) Does the sole have a bit of bounce? Yes No (This helps prevent jarring to your foot) Does the sole have some grip? Yes No Does the heel have a rounded edge? Yes No (Sharp shoe edges can slip easily on wet or shiny surfaces) If you circled No to any of these questions, you may be at increased risk of falling. Please take this checklist to your Podiatrist, family doctor or practice nurse so that you can discuss ways to reduce the risks.
Therapy Professionals Ltd friendly physiotherapist can help, just contact us on phone 03 3811741 or email: [email protected] to make a time. Ref: Adapted from Public Health Division © Health Department of WA 1999 SOYF What can you reasonably expect of your physiotherapist in aged care?  Aged care residential services have changed greatly, expectations are greater and funds are less generous. Once many aged care facilities provided maintenance and rehabilitation physiotherapy services, now the budget doesn’t allow for rehab. What is Maintenance Physiotherapy - assessment, planning and review of:
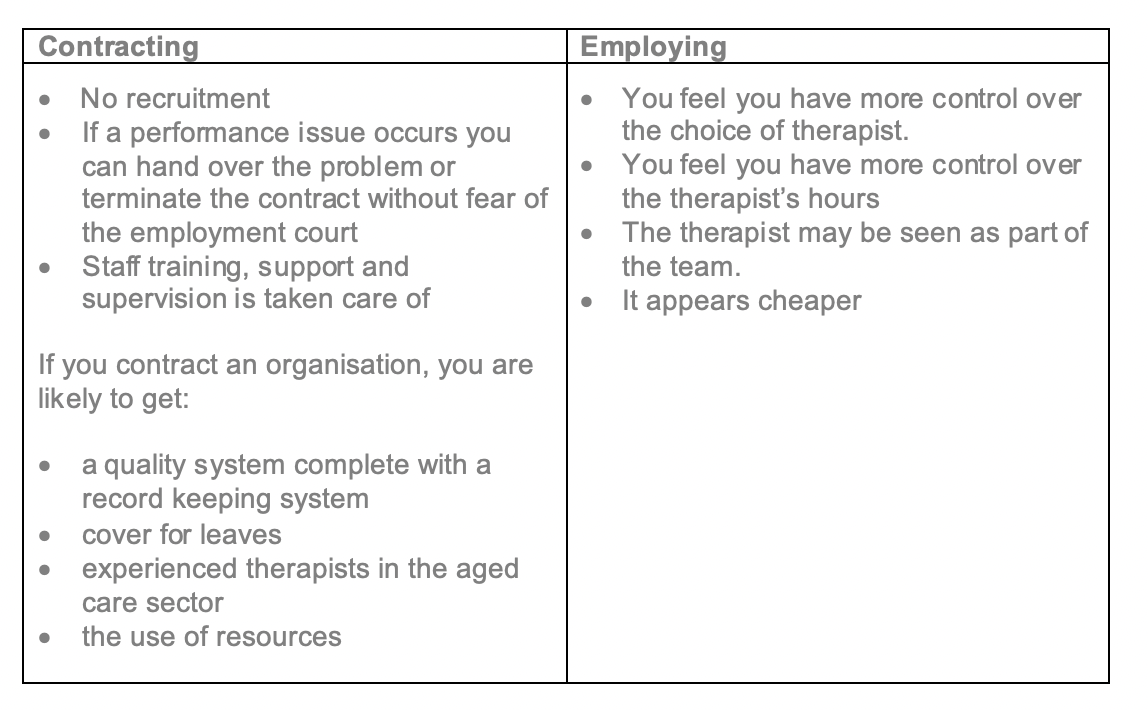
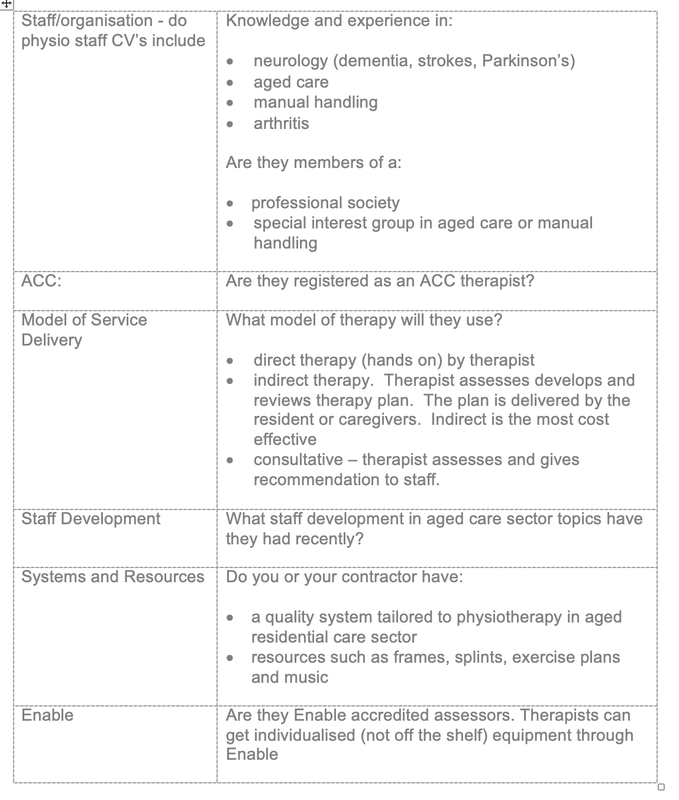
The implementation of most of these plans will be done by care staff not the physiotherapist. So what happened to rehabilitation? Most facilities can’t afford the intensive hours of individual physiotherapy to rehabilitate someone following a stroke or recovering from a fractured neck of femur. How might this be managed? Strokes – either gain service from the Health NZ. OR many families can pay privately for a burst of intensive physiotherapy. Fractured Neck of Femur – Treatment is subsidised by ACC for 12-16 treatments. Most physiotherapists will require a co-payment. The facility or family would need to pay for this. Individualised Wheelchairs? These can be very time consuming at up to 6-8 hours per individual. We would suggest it’s not the most equitable use of your budget. Health NZ has a wheelchair and seating team, a physiotherapist can access this. However there is often a long waiting list. OR your clients can pay privately for a physiotherapist to prepare for and organise an appointment at the Enable equipment clinics. How do you know your therapy services are value for money? It is hard to know if you’re purchasing quality. What can you, the purchaser of services, do to ensure you are purchasing good quality, value for money services? The same due diligence is needed when employing or contracting for physio services as you use for any of your staff. Things to consider  Efficiencies are made with experience, good systems and the use of an indirect therapy model. An expert in any area may cost more per hour however their experience brings savings in time, supervision and training costs as their knowledge is deep and at their fingertips. They get more work done per hour. Employing vs Contracting Many employers when deciding on whether to contract or employ make the mistake of comparing the contract hourly rate with the hourly rate. They forget to include other costs of employing eg leaves, ACC levies, staff training, support and supervision, insurances, Kiwi saver, general management and administration costs. When comparing costs the general rule of thumb is to multiply the recommended hourly wage rate by 2.5 and you get a rough estimate of the cost of employing. Additional costs to consider are:
 Comparing potential contractor’s price
Check:
|
AuthorShonagh O'Hagan Archives
July 2024
|



 RSS Feed
RSS Feed