 Making Sense of our Senses To understand our environment we receive information through our senses, our brains process the information, and respond, helping us do our everyday activities. Most of us are familiar with the five senses – sight, hearing, smell, taste, and touch. However, there are two other senses we use:
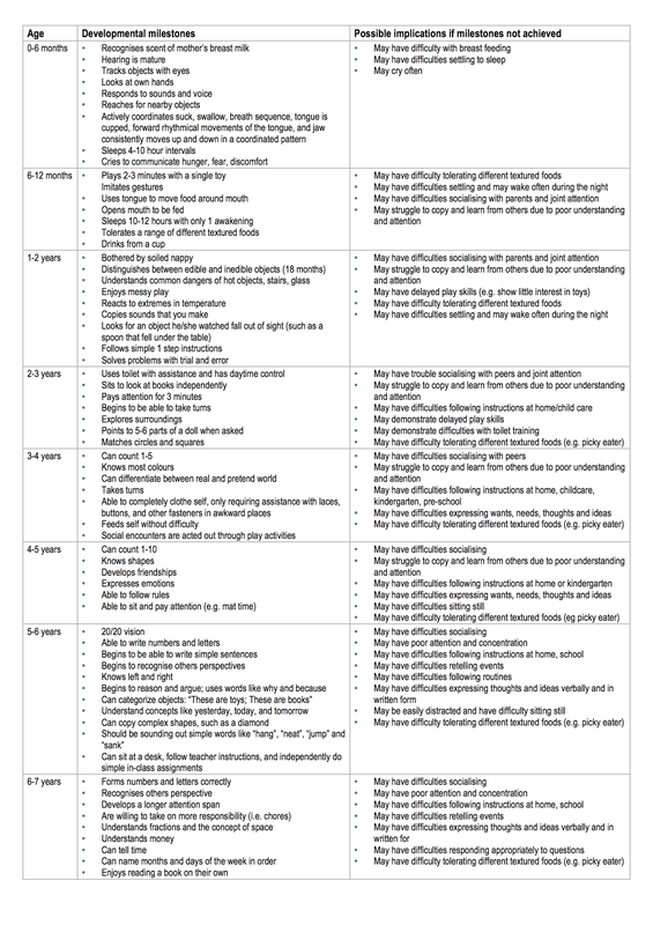
We all experience sensation in our own unique way, some of us may overreact while others underreact to sensory input. Someone may find a certain smell nauseating while others don’t even notice it or they may find a fabric irritating on their skin while others don’t. People who overreact to sensory input will tend to avoid the sensory experiences. A person who underreacts will often seeksensory experiences, eg loud music or rollercoster rides. Children with autism or learning disabilities often have issues receiving, processing or appropriately responding to one or more of their senses, making it hard to function in everyday life. Our ability to use this information matures over childhood in an orderly and predictable manner. There may be some variation in the speed with which children acquire each milestone. If milestones are not reached there may be implications for the child’s health, wellbeing, learning and understanding of the world around them. The chart below has some developmental milestones and the behaviours, which may result if the milestones are not acquired. If you have a child who has not yet mastered the milestone at their current age, contact our friendly Occupational Therapists. 5Chart designed by Australian Curriculum, Assessment and Reporting Authority.
This chart was designed to serve as a functional screening of developmental skills per age group. It does not constitute an assessment nor reflect strictly standardised research. If a child is found to have trouble with sensory input there are things we can do to help, just contact us: Phone: 03 3775280 or email: [email protected] Oral Care For those without teeth or are tube fed  Many people mistakenly think because they, or the people they are caring for, have no teeth or are fed via tube, there is no need to clean their mouths. This is simply not true. Oral and dental diseases can be a contributing factor to pneumonia as the levels of bacteria in the mouth and saliva are increased. If saliva or food/fluid contains these bacteria and enters the lungs (aspiration), it can increase the risk and severity of chest infections. If oral care is not maintained oral and dental disease is more likely and so are chest infections, including pneumonia. Is oral care for everyone? Yes. Each individual should have a plan for oral care including anyone without teeth and even those who do not eat/drink orally (ie are tube fed). Why is oral care important?
How often?
Equipment that can assist with oral care:
How to do oral care/tips: Sometimes it can be hard to remember to do oral cares.
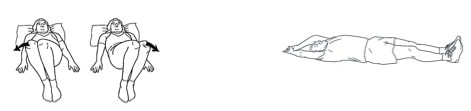
If you are having any trouble implementing oral care, please don’t hesitate to seek help either from an oral hygienist, dentist or our friendly Speech Language Therapists. For advice especially for those with disabilities talk to our friendly Speech Language Therapists who are experienced with disabilities. Just contact us at Therapy Professionals Phone: 03 3775280 Email: [email protected] Website: www.therapyprofessionals.co.nz Beat morning stiffness If you have arthritis you will probably find it difficult to get moving in the mornings. You’re not alone. Early morning stiffness in the joints is common for people with Arthritis. It pays to wake your joints and muscles up slowly before you rise in the morning. Our friendly Physiotherapists suggest you try this daily routine before getting up in the morning Do each of these exercises 6 times in this order. While still in bed: 1. Wiggle our feet up and down vigorously. 2. Bend your legs up and down, one at a time 3. With both sides bent, rock gently from side to side. 4. Stretch both arms above your head (if necessary help weaker arm with stronger one) 5. Lie on your back with knees bent, lift your bottom off the bed While sitting on the edge of the bed: 6. Straighten each leg one at a time. 7. Tuck chin in gently turn your head to look over your right shoulder. Repeat on your other side. Get onto your feet, PAUSE, and get your balance before continuing with your day.
These exercises will help your joints and muscles ease into the day. Take it easy when you change from lying to sitting or sitting to standing as you may experience dizziness which can result from rapid changes of position – lying to standing or sitting to standing. Make a point of moving regularly during the day and even better join one of our Arthritis exercise classes. To find out where they are contact our office.. If you wish to have some additional advice on managing your Arthritis our friendly Physio’s can help. Just contact us: Ph: 03 3775280 Email: [email protected] Compiled for you by our friendly physio’s. Therapy Professionals Ltd, PO Box 7807, Christchurch 8240 Phone: (03) 377 5280 Fax: (03) 377 5281 Email: [email protected] Website: www.therapyprofessionals.co.nz  Seating Advice for Residential Care The frail elderly and disabled in care spend much of their day sitting, often in unsuitable chairs, which restrict their mobility and cause them to adopt slumped postures. Correct seating allows clients to:
When a resident has difficulty rising from an armchair, consider the seat height, depth, width, slope and firmness, and the armrest height. When choosing an armchair for your residents consider these things: a) Height: For comfort and ease of getting out of the chair:
b) Width: There needs to be a space of 2-3 fingers either side of the body to allow wriggle room and to keep the armrests comfortable. c) Depth: The depth needs to ensure a good upright posture and for ease
d) Back rest: needs to:
e) Arm rests: need to:
f) The chair surface needs to:
 Residents come in all shapes and sizes, we recommend Residential Providers
Choosing wheeled chairs For staff safety when choosing wheeled chairs, ensure the wheels are larger enough to push easily on all floor surfaces while allowing the ambulant person’s feet to rest on the floor so they can stand easily. If your current wheeled chairs are hard for staff to push, see if you can get larger castors or wheels, or check that fluff is not restricting the wheels.. Couches We don’t recommend couches as they are harder to get out of and harder to assist someone to stand. If you need any advice on purchasing suitable chairs our friendly physios and occupational therapists can help, contact us as follows: Ph: 03377 5280 Email: [email protected] Website: www.therapyprofessionals.co.nz  Osteoporosis and Diet Therapy Professionals Ltd’s Dietitian reports on Osteoporosis and Diet Bone is a living tissue that is continually remodelled and rebuilt throughout a person’s life. Calcium deposits make bones strong. Eating a balanced diet that includes calcium rich foods is important in maintenance of bone strength. As the body grows, bones become stronger, peaking in mass at about age 30. After this, bones lose calcium as part of natural ageing both in women and men. Oestrogen helps to keep calcium in bones, so when levels drop at menopause, women lose calcium from bones more rapidly than men do. Things that reduce bone strength: Smoking Among the many health benefits of stopping smoking, this will improve absorption of many nutrients from the diet, including calcium. Alcohol Four or more alcoholic drinks a day can reduce calcium uptake by the bones despite dietary intake. Weight Being overweight may add stress to bones, however generally leads to a decrease in mobility and weight bearing exercises. Research shows being underweight or having a slight frame also can increase the risk of osteoporosis.  How to keep my bones strong? Exercise Regular weight bearing exercise where some strain is placed on the bones builds up bones in young people, and slows down loss of bone density in older people. Weight bearing exercise requires your muscles to move against gravity eg walking, jogging and playing sports (swimming, cycling and rowing are not weight bearing activities).  Sunshine Vitamin D is needed for calcium to be deposited into bones. Sunshine (ultraviolet light) is needed for the body to produce its own Vitamin D. If exposure to sunshine is limited during aNZ winter especially in the south island, food sources of Vitamin D are important. These include fish oils, sardines, tuna, eggs, butter and margarine and liver. Healthy diet A diet rich in calcium and a variety of foods from the four food groups - fruit and vegetables, breads and cereals, meat or meat alternatives, and milk and dairy products ensure good general health. How do I achieve a healthy calcium intake Adult men and premenopausal women need 800mg of calcium per day. Adult men and premenopausal women need 1000mg of calcium per day. Post menopausal women (over 51 years) and men over 70 years 1300mg per day. The table below shows how to achieve a healthy calcium intake. Dietary Supplements
The preferred source of calcium is from food and the preferred sources of Vitamin D are sunlight and food. Food also contains other important nutrients such as phosphorus, zinc and magnesium, protein and other vitamins. Vitamin D If you are unable to get outside regularly you may need a Vitamin D supplement. Calcium If you don’t like, or can’t eat calcium rich foods, calcium supplements may be necessary. Discuss with your doctor whether dietary supplements are necessary, and which type is best for you. Therapy Professionals Ltd has dietitians available who are able to provide information to groups or individuals on many aspects of nutrition. Just contact us Phone: 03 3775280 Email: [email protected] References Arthritis Foundation of NZ and DAB ‘Your Bones, Your Future’ Arthritis Foundation of NZ and DAB ‘Look after dem bones’ Mann, J, Trusswell S, ‘Essentials of Human Nutrition’ 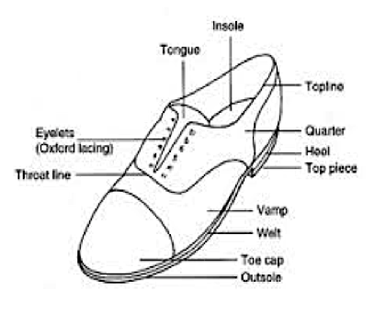 Footwear Matters Here at Therapy Professionals we know the value of comfortable feet. Good footwear is important throughout life, however, as we age it becomes even more important. Poor footwear can cause foot, back and knee pain, and discomfort from corns, calluses and fungal infections. High heels and sloppy fitting shoes can affect our balance and walking, making us prone to falls. Any of these make us less inclined to walk affecting our health, wellbeing and independence. To avoid pain and discomfort caused by ill-fitting shoes and to maintain your fitness and independence as long as possible, just follow this advice from our friendly Physiotherapists. As we age our feet change shape and become larger so it’s important to get your feet re- sized when you are buying new shoes. Here are some tips on buying shoes: The essential components of good shoes are that they:
The shoe
If you need advice about the best type of footwear for you, Therapy Professionals friendly Physiotherapists can help, just contact us Phone No: (03) 377 5280 Email: [email protected] Website: www.therapyprofessionals.co.nz  Can People on Modified Diets have Food Treats? At any celebration - Christmas, Birthdays and Easter, it’s common for us to have food treats like sweets and nuts. Unfortunately we notice a great increase in choking incidents and chest infections caused by aspiration over holiday seasons, because people forget these treats are food. Yes, people on modified diets can have treats however they need to be modified in the same ways as their usual foods. In order to help you keep your clients safe from choking and chest infections our Speech Language Therapists have come up with a few alternatives for you to try. Pureed diet: (smooth and uniform texture)
Minced and Moist diet: (needs to be very finely cut or mashed). All options suggested for a pureed diet plus:
Easy to Chew diet: (must be able to be easily and cleanly cut with the side of a fork) All of the options in pureed and minced and minced and moist plus:
This list is not a complete list; you may come up with some of your own ideas as long as what you’re giving your clients is the correct texture prescribed. If you require any assistance, our Speech Language Therapists can help. Just contact us: Phone: 03 377 5280 Email: [email protected]  Assisting someone to walk Keeping older people mobile and on their feet is good for families, their carers and the older person. The more people can do for themselves the less physical strain there is on the carer. Often carers try to help older people get up from sitting and walk by hooking the older person under the arm, which could easily damage the older person and the carer’s shoulders. The other mistakes we often make are:
If you want to assist an older person walk, first we need them to stand. Just follow the guidelines:
- shuffle their bottom forward in the chair - place legs shoulder width apart - tuck feet under chair - lean forward, feet on the floor, nose over toes
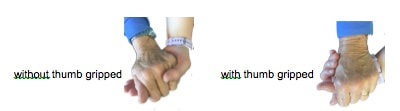
- on the count of “Ready, steady, stand” ask them to push up through their hands and feet to stand Walk the person while holding them with your arm across their back and hand on their bottom or hip. Their shoulder should be sandwiched firmly between your shoulder and hand. They may use a walking stick or walker. You may wish to use a hand grip instead of the shoulder sandwich hold. Hand grip Have your hand open upwards and allow the person to grab it. If you can avoid them grabbing your thumb do so especially if the older person has dementia. |
AuthorShonagh O'Hagan Archives
July 2024
|






 RSS Feed
RSS Feed