 When communicating becomes difficult When someone’s age, disability, injury, or illness is making communication difficult, it can make life very frustrating. Here are some helpful tips to improve communicating with someone who is struggling to communicate:
Therapy Professionals friendly Speech Language Therapists can help make communication easier, just contact us: Phone: 03 377 5280 Email: [email protected]. Some helpful hints for exercise class leaders taking classes for older people  Keep in mind when taking exercise classes these important points:
Hints for the class
 Specific Conditions Arthritis - Osteo and Rheumatoid
Rest is best – start exercising as these symptoms subside
Osteoporosis
Total Hip Replacement Those movements to be avoided over the first eight weeks (all patients have been told in hospital)
Total Knee Replacements
 Hints for Stair Climbing – for troublesome hip or knee
“Up to Heaven, down to Hell”  Getting down to the floor and up Down to the floor - use a chair – seat to lean on
Up from the floor - get on all fours next to a chair
 Chest conditions and shortness of breath
Specific Movements to Stress
exercise – try slowly up and down (as long as knees are not sore)
- encourage using support (a chair or wall) if confidence is lacking - Or holding each other! - progress to not holding on for these exercises Suggestions - walk on tip toes - “heel-toe” walk - heel walk - exercises standing on one leg - walking backwards Arthritis There are over 100 types of arthritis. Each type of arthritis is different, therefore, needs different treatment. Arthritis may cause pain, stiffness, swelling, tenderness or inflammation of the joints or affected areas. It can also prevent some movements which are necessary for the activities of daily living. It is important that people should try to learn as much as possible about this disease so that they may be able to understand how to control it. Did you know that:
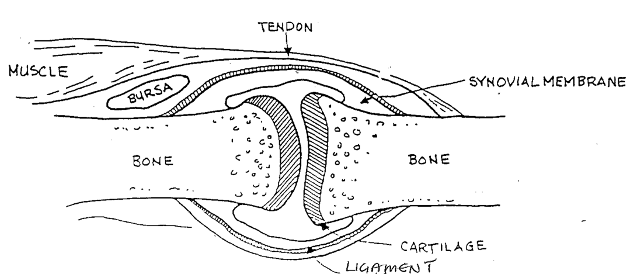
Functional parts of a joint: Cartilage: A tough material that cushions and protects the ends of bones. (Example of arthritis in this part: osteoarthritis.) Synovial membrane: A thin layer of tissue which surrounds the joint and contains and produces a lubricating fluid (synovial fluid). This fluid oils the joint and is also responsible for keeping the cartilage healthy. (Examples of arthritis in this part: rheumatoid arthritis, gout.) Bursa: A small sac located near the joint which contains a lubricating fluid. This sac allows smooth movement of muscle across muscle and tendon across bone. (Example of inflammation of this part: bursitis.) Muscle: The muscles are elastic tissues that work together to move the bones by contracting and relaxing. (Example of involvement of this part: fibrositis.) Tendon: Tissue fibre which attaches muscle to bone. (Example of involvement of this part: tendonitis.) Ligament: Tissue fibre which attaches bone to bone. (Example of arthritis in this part: ankylosing spondylitis.) OSTEOARTHRITIS Also called: Degenerative joint disease Degenerative arthritis Osteoarthrosis What is it? Osteoarthritis is a degenerative disease which most often affects the ‘weight-bearing joints’ ie ankles, knees, hips, spine. The cartilage breaks down, tears, or rips and leaves the bone surfaces without a cushion. How do I get it? The cause of arthritis is not definitely known, but it can be caused by one or more of the following factors:
How does it affect me? Bony growths or ‘spurs’ may appear in the affected joint, causing intense pain and limited movement. Due to the lack of cartilage, bone surfaces rub together resulting in pain and limited movement.  RHEUMATOID ARTHRITIS What is it? Rheumatoid arthritis is a disorder which involves many of the body’s systems and often affects the toes, ankles, knees, shoulders, elbows and fingers. The synovial membrane which lines the joint, becomes inflamed. About one person in 100 of the population have rheumatoid arthritis, and two to three times more women do than men. How do I get it? There is no known specific cause of rheumatoid arthritis, but the latest theories suggest that it develops from a viral or bacterial infection. It is an auto-immune disease, which means your body is attacked by its own defence mechanism. How does it affect me? Rheumatoid arthritis causes many problems because it works on many of the body’s systems. Some of the problems are:
Reference: Healthy happy ageing: a positive approach to active living
Yvonne Wagorn, Sonia Théberge, Dr William R Orban Care Home / Aged Care Checklist Care homes and aged care facilities vary considerably and it’s important to get the best fit for your family member. It’s often hard to know what to look for. Here’s a checklist from the Aged Advisor 2023 edition which may help you decide. Consumer also put out a good checklist a number of years ago. https://d3c7odttnp7a2d.cloudfront.net/assets/8159/Rest_Homes_checklist.pdf Use this as a reference. You may wish to either tick if it applies, add ‘yes’ or ‘no’ or give a personal rating from 1-5 to help compare your options. from Aged Advisor www.agedadvisor.com Questions: Facility and Care What are the levels of care offered? (eg rest home, dementia) Is there an ORA/Entry Price? (eg $230,000) Is there a Premium Room Fee? Daily, weekly, 28 days? (eg $30 per day) Is a GP on call 24/7? Is a registered nurse on 247? (eg yes, yes) Overall atmosphere in the care home? (eg light, warm, homely) Last DHB Audit result? (eg 48 months) Individual Room Do rooms appear clean and homely? Is there plenty of natural light? Was the temperature comfortable? Adjustable heating in the room? Can residents bring own furniture? Do the rooms have an ensuite? Social Are residents normally in the lounge or own room? Can they choose? Is there a weekly activities programme? What are the activities like? Is there a Physio, Occupational or Diversional Therapist? How many hours per week are they available? Is there spiritual care available? How often? Within the home or externally sourced? Overall atmosphere in the village? Were staff / management approachable / friendly? Did residents appear relaxed and happy? Location Near friends, family? (eg yes, yes) Nice green spaces? Multiple quiet spaces / gardens? Ground floor or multi-level? Easy parking for visitors / family? Meals Do meals look appetising? What do other residents / visitors say about food? Are there tea / coffee making facilities for residents? Are special dietary needs met? Is there any additional cost? Reference: Aged Advisor 2023 edition
|
AuthorShonagh O'Hagan Archives
July 2024
|

 RSS Feed
RSS Feed